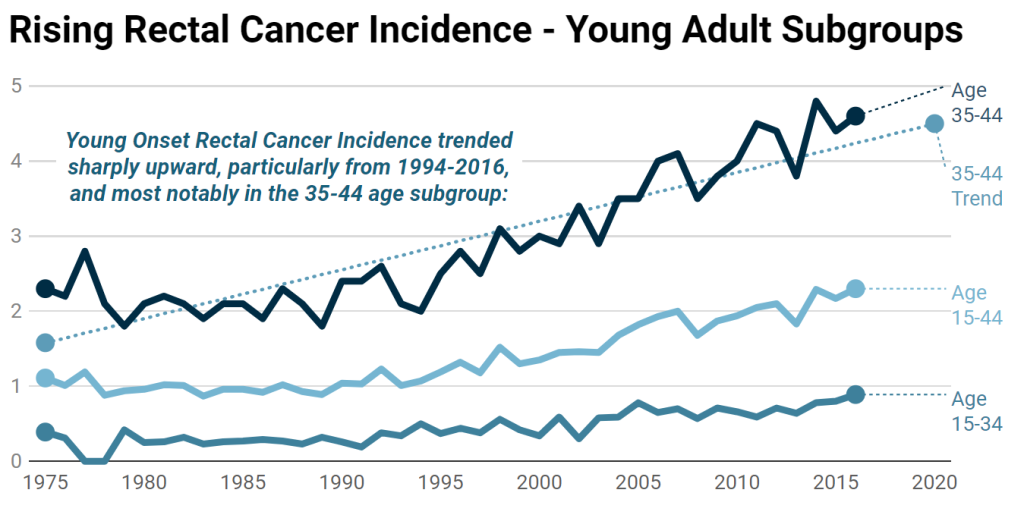
Colon cancer is one of the most common cancers worldwide, and its incidence has been rising over the past few decades. Notably, rates in adults under 50 years increased by 22% between 2000 and 2013. The American Cancer Society projects an estimated 53,010 individuals will die due to Colorectal Cancer in 2024, this is an increase compared to last year’s numbers. CRC is now the leading cause of cancer-related death among men under 50 and the second leading cause among women in the same age group. Younger patients often present with more advanced and aggressive disease, influenced by a combination of biological differences, genetic factors, and delayed diagnosis.
Why is colon cancer increasing in young adults?
The answer is not clear however there are various factors that are suspected to play a role including lifestyle, genetics, biologics.
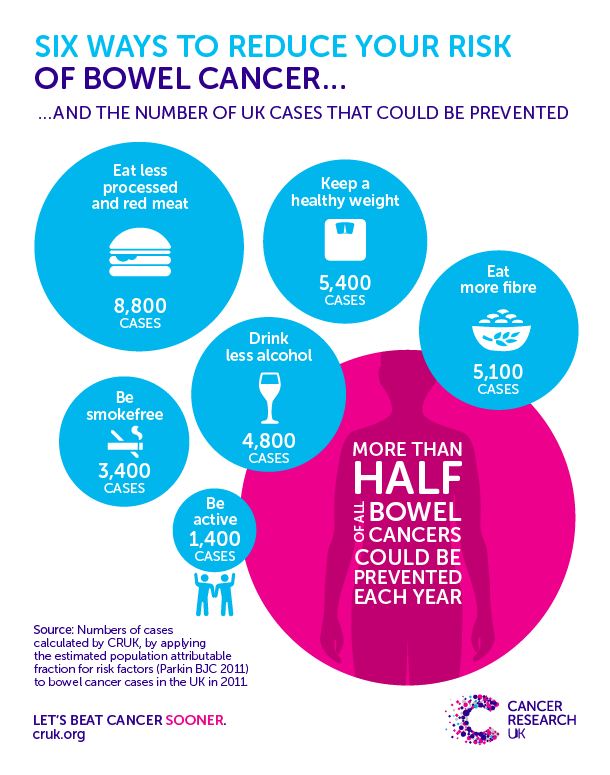
Diet: The Western diet is characterized by high intake of packaged and processed foods, excess sugars (especially fructose), and elevated dietary salt. It often includes large amounts of processed and red meats and high-fat dairy, which can introduce carcinogens and trigger inflammation. Additionally, this diet is typically low in fiber from fruits, vegetables, and whole grains, which are essential for healthy digestion. These dietary patterns contribute to inflammation and increase the risk of chronic conditions. The gut microbiome, a complex ecosystem, plays a significant role in overall health. Dysregulation in gut microbiota has been linked to chronic diseases, including obesity, hypertension, diabetes, inflammatory bowel disease, and even cancer.
Sedentary lifestyle: Physical inactivity may contribute to cancer by promoting insulin resistance, increasing the risk of obesity, and increasing inflammation overall. Moderate exercise can support digestion and improve gastrointestinal function.
Genetics: Genetic factors can significantly influence colon cancer risk. A family history of colon cancer suggests a higher likelihood of developing the disease. Some genetic conditions that increase risk include Lynch syndrome, familial adenomatous polyposis (FAP), Peutz-Jeghers syndrome, and DNA mismatch repair mutations.
Smoking/Alcohol intake: Exposure to carcinogens and inflammation-inducing molecules from alcohol and tobacco/e-cigarettes has been linked to colon cancer.
What can you do to stay healthy?
Dietary and lifestyle changes can make a significant impact.
- Stop Smoking: Tobacco smoke, including e-cigarettes/vaping, can increase risk of not only lung cancer but other cancers as well due to the exposure to carcinogens.
- Exercise: Sedentary lifestyle has been associated with greater risk of developing colorectal cancer
- Increase fiber intake: Eating more whole grains, fresh fruits, and vegetables while reducing processed food intake is recommended.
- Drink responsibly: Alcohol consumption is associated with an increased risk of developing cancer
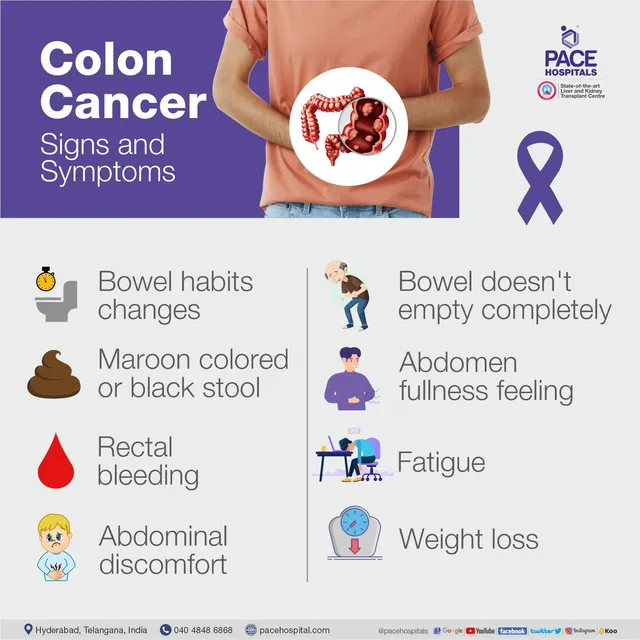
What are some symptoms to watch for?
Even if you are young, it is important to know when to seek medical care, especially if you are noticing the following symptoms:
- Changes in bowel movements: New onset constipation, inability to completely empty bowels, or loose stools lasting more than two weeks should prompt an evaluation by a medical practitioner.
- Rectal bleeding: Bright red blood in your stool/in the toilet after a bowel movement needs medical care. Dark/black tarry stools may also indicate bleeding.
- Stool changes: Tumor-related obstruction can lead to thin, narrow, ribbon-like stools.
- Unexplained fatigue: Blood loss from colon cancer can lead to anemia, causing fatigue and weakness.
- Weight loss and abdominal pain: Unintentional weight loss and persistent abdominal pain should not be ignored.
Should you get a colonoscopy?
Screening can be lifesaving. There are several ways that a patient can be screened for colon cancer however the gold standard test is a colonoscopy. A colonoscopy is a procedure where a flexible scope is inserted through the rectum to examine the colon while the patient is under conscious sedation. In 2021, the U.S. Preventive Service Task Force (USPSTF) lowered the recommended starting age for screening from 50 to 45 due to the increasing incidence of early-onset colon cancer.
If you have a history of colon cancer, it may be recommended for you to undergo a colonoscopy at the age of 40 years or 10 years before the age when your family member was diagnosed, whichever is earlier. Screening frequency may vary based on your risk factors and any findings from prior colonoscopies. Please talk to your doctor to discuss your risks and your screening options to determine the best approach for you.





